Development Of Congenital Heart Defect Treatment- The Key Milstones
February 7, 2024 | Contributed by Dr. R. Vijayakumar
Congenital Heart Defect Treatment has come a long way over the last many decades. While many decades ago a child born with a congenital heart defect was doomed to severe disability or death, in today’s times, most children born with a heart defect can live near normal lives well into adulthood, with just a single intervention. Timely diagnosis and treatment being the key.
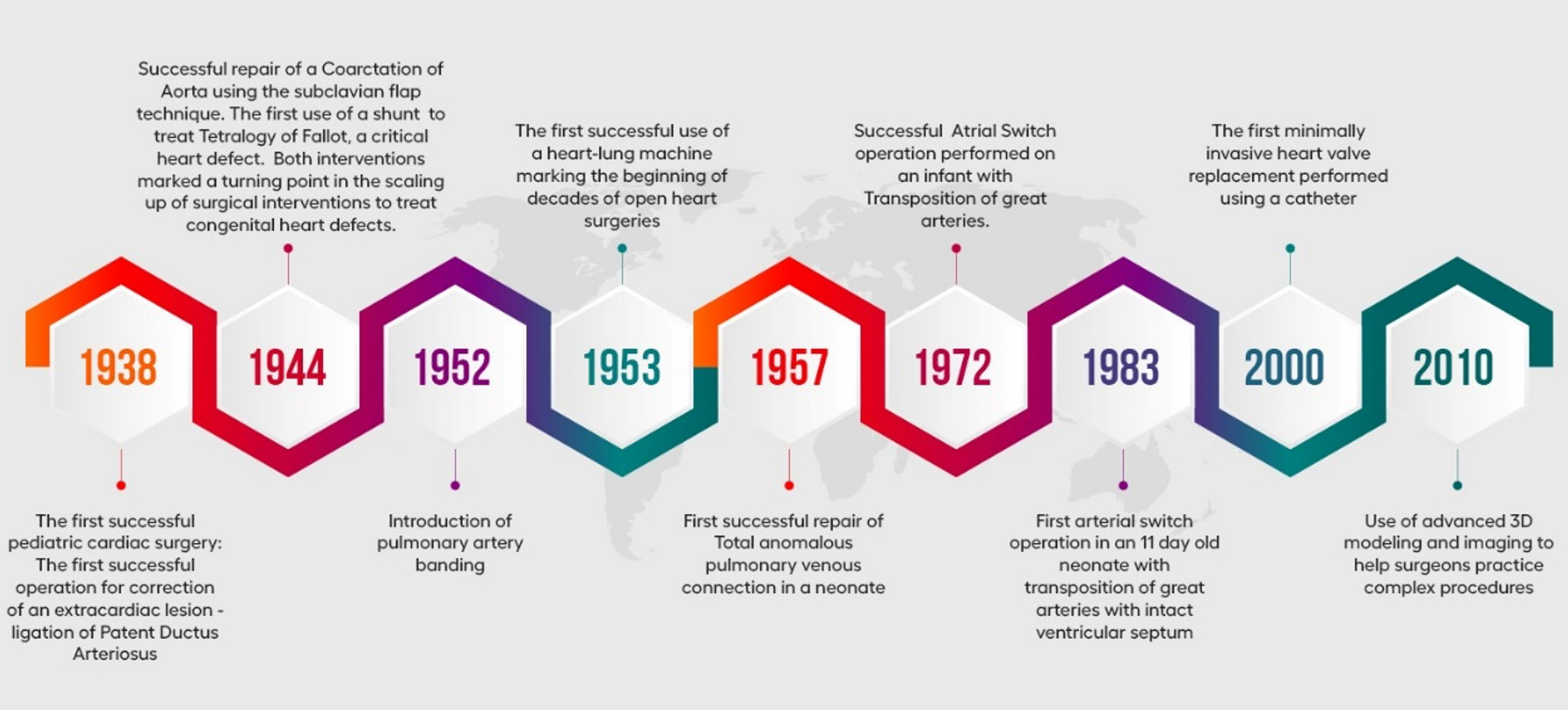
However, this has taken years of development. Following is a summary of the key milestones in the development of congenital heart defect treatment.
The 1930-1950s.
Pediatric cardiac surgery began with first successful operation for correction of an extracardiac lesion – ligation of Patent Ductus Arteriosus. This was accomplished by Dr. Robert Gross and Hubbard on August 8, 1938 at the Children’s hospital in Boston. The seven-year-old girl who underwent the procedure lived on to be a great-grandmother.
Six years later on October 10, 1944, Crafoord and Nylin at the Karolinska hospital in Sweden, successfully repaired a Coarctation of Aorta using the subclavian flap technique. In the same year, on November 9, Aldred Blalock, Helen Taussig and Vivien Thomas carried out the first subclavian artery to Pulmonary Artery Anastamosis to palliate cyanosis – to treat Tetralogy of Fallot, a critical heart defect. These two interventions marked a turning point in the scaling up of surgical interventions to treat congenital heart defects.
In 1952 Muller and Dammann introduced the pulmonary artery banding to protect the pulmonary arterioles from developing pulmonary vascular obstructive lesions, a consequence of increased pulmonary blood flow and pressure.
The Challenges and lessons Learned
The challenges during late the forties and early fifties was how to gain access to the interior parts of the heart. Several ingenious measures were proposed and performed. Although useful in some patients , these technique were inadequate for the repair of most intracardiac defects.
In the early fifties, Boerema and associates in Amsterdam, Bigelow and colleagues in Toronto, Lewis an Taufic at the university of Minnesota began to use total body hypothermia. Their purpose was to lower the metabolic demand of the body tissues especially the central nervous system. This will allow for longer period of caval occlusion.
In 1933 John Gibbon, at that time a surgical resident at Jefferson university, while on a clinical rotation at the Massachusetts General hospital in Boston, witnessed the death of a young woman from a pulmonary embolus. Gibbon recognized that removal of the saddle embolus could have saved the life of this of this other- wise healthy young woman. Despite little support from the senior staff at the Massachusetts General hospital, Gibbon obstinately persisted in developing an artificial heart lung machine. After many clinical trials, twenty years later on May 9, 1953, he succeeded in closing the atrial septal defect in a young women using a screen oxygenator of his own design and a roller pump. This was the first open heart surgery performed by connecting the patient to Cardiopulmonary bypass machine. This was a big stepping stone to decades of open-heart surgery.
During the same period Dr. C. Walton Lillehei performed complete repair surgery for ventricular septal defect, Tetralogy of Fallot, Complete atrioventricular canal defect using controlled cross circulation technique. Although this technique is useful in performing the congenital surgery successfully, it has its drawback of subjecting a healthy donor to the risks of anesthesia, anticoagulation, and cannulation of important veins and arteries with added thread of air embolism made this technique less than practical for routine use.
John Kirklin accompanied by Mr.Richard Jones, an engineer from Mayo clinic paid a visit to Gibbon’s laboratory to study in details his heart -lung machine. Kirklin and Jones succeeded in improving and simplified the Gibbon’s screen oxygenator, called from then on Mayo- Gibbon pump oxygenator. In the mean time, Richard DeWall at the university of Minnesota developed a very simple, easy to assemble and to use, bubble oxygenator. Subsequently open heart centers spread rapidly, first in the united states and then throughout the world. Beginning of all open heart operations were indicated for the repair of congenital cardiac lesions.
During 1950’s and 1960’s the prevailing impression among doctors and some child heart foundation was that open heart operations were poorly tolerated by the very young neonates and infants. Therefore, the symptomatic neonates and infants were first subjected to palliative procedures, then staged to the definitive intracardiac repair after 5 to 7 years. This method of care has several disadvantages such as need of redo- surgeries and its complications. Hence the primary repair in these small kids had been developed slowly in late sixties. Horiuchi and co-workers, Hikasa and associates in Japan , Barrot – Boys and colleagues in New Zealand started to obtain good results with primary repair in infants.
In 1957 Cooley and Oschsner first performed the first successful repair of Total anomalous pulmonary venous connection repair in a neonate. In the same year Edgar Davis ligated the left coronary artery for Anomalous origin of left coronary artery from pulmonary artery. Although this procedure is not followed now.
The 1960s – 1980s.
These decades saw more sophisticated techniques being performed on neonates and infants. In 1972, the Atrial Switch operation was successfully performed by on an infant with Transposition of great arteries. The procedure helped correct the position of the two main arteries. On January 2, 1983 Jatene performed the first arterial switch operation in an 11 day old neonate with transposition of great arteries with intact ventricular septum.
1990s- the Current Time
In the current era, congenital heart defect treatment has advanced and improved significantly. Techniques have improved to handle the perioperative care as well as use minimally invasive methods to treat congenital heart defects. in 2000 the first minimally invasive heart valve replacement was performed using a catheter heralding a new phase in the treatment of congenital heart defects. Development of conduits – valved and non valved have benefited many children with complex congenital problems. Hybrid procedures ( collaboration of interventional cardiology and surgery) has enhanced the treatment care to these needy children now days. 3D modelling and imaging has allowed surgeons to prepare for complicated procedures.
In Future the area of interest will be genetic engineering to develop the biological tissues in vitro to be used for complex surgery. In vitro fetal surgery during the gestational period will be the upcoming field in the treatment of congenital heart defect.
References:
- Congenital Heart Disease : A surgical – Historical Perspective – Aldo Castaneda,( Ann Thorac surgery;79:S2217-20)
- The Early history of congenital Heart Surgery: Closed Heart Operations – John A. Waldhausen ( Ann Thorac Surgery 1997;64:1533-9)
Dr. R. Vijayakumar
Director- Center for Pediatric Congenital Heart Disease, G. Kuppuswamy Naidu Memorial Hospital

