Congenital Heart Disease: The Indian Context
March 30, 2022 | Contributed by Dr Swati Garekar
“Can babies really have heart disease?”
A common enough question casually addressed to many pediatric cardiology practitioners, because lack of awareness makes it unbelievable for so many families that Congenital Heart Disease treatment is needed for children. But indeed, babies do have heart disease. In fact, most texts state a figure of 8 in 1000 babies having one or the other problem of the heart. This is far more common than cleft lip/palate that are seen in 1/1600 babies.
Heart disease in babies is not cholesterol plaques in coronary arteries causing chest pain and heart attack. Rather, babies have birth defects of the heart called Congenital Heart Defects or more commonly as CHD. The heart is formed in the first 2 months of becoming pregnant- implying that when a woman discovers and gets around to proving that she is pregnant, the heart of the fetus is already formed.
For multifactorial reasons, due to poorly understood work in progress, sometimes there is a malformation in the heart — there is a hole in the walls inside the heart, or the valves don’t open or close completely, or the vessels connect to the wrong chamber or the chamber itself is poorly formed.

Most of the time, the malformed heart doesn’t interfere with the baby’s growth until after the baby is born. A critical malformation of the heart makes a newborn baby really sick to the point of being life-threatening. The symptoms of such a baby are dull, inactive appearance, cool to touch, dusky appearance, rapid breathing and no interest in feeding. An alert doctor will suspect infection or CHD in such cases. The way to diagnose a CHD is to get an echocardiogram-an ultrasound of the heart, by a pediatric cardiac specialist. Congenital Heart Disease treatment of each CHD varies from surgery to an intervention in the Cath lab. There is very little room for medications in heart disorder treatment. The outcome of the majority of the CHDs when intervened at the correct time, is very good. Though long-term follow up in some pediatric cardiac OPD cases is essential.
Status of CHD in India
In India, the exact numbers of babies suffering from heart defects is unknown: the number of studies is less, only cases that reach the hospital are counted, an unknown number of affected babies die before reaching the hospital or are living with the disease, undiagnosed. According to a 2018 paper[1] by Dr A Saxena, pediatric cardiologist at AIIMS, New Delhi, the number of centres catering to such babies is very inadequate: one centre per 160 lakhs population in Asia compared to 1.2 lakhs population in North America. It is estimated that 2.4 lakh babies are born with heart defects every year in India, of which ~43,000 will need heart surgery or intervention in the first year of life. Only 11,000 surgeries/interventions were performed in the first year of life in a particular year (2016-2017) in India as per available data. So there is a gap between supply and demand, that only worsens with each passing year as cases accumulate.
Challenges faced by pediatric cardiac specialists in diagnosing and treating CHDs

- Fetal echocardiogram
The first chance to diagnose CHD comes during pregnancy: a fetal (unborn baby) echocardiogram can be done at 4.5 to 5months. This test can diagnose most major CHDs, but not all.
A diagnosis at this point helps the would-be parents make informed decisions and plan for their unborn child. A fetal echo is labor intensive, time consuming and costly. Hence there are specific indications to do it. The best option is for the radiologist to include special views of the fetal heart in the anomaly scan of the fetus. A suspicion that the fetus has a malformation can then prompt a referral for a fetal echocardiogram. This system works well in the developed world such that they are able to diagnose most of the major CHDs before birth. A baby doesn’t have to develop a life threatening state in order to get diagnosed after birth.The challenge in India, is that all aspects of antenatal care (pregnancy care) is not available. So, many pregnant women do not even get the anomaly scan. Further, many who do, have scans that do not include the screening views of the heart.
- Newborn care
After being born at a hospital, a baby is examined by a doctor prior to discharge home. This is another opportunity to screen for the general health of the baby. A simple pulse oximeter check can also help identify new-borns whose hearts have certain major malformations that render a lower level of oxygen in the blood. A pulse oximeter is the same instrument made ubiquitous during the ongoing COVID-19 pandemic – a must have for oxygen levels check in homes across the country. The screening of all new-borns prior to discharge home is practised as a rule in most developed nations and is simple and cost effective
- Echocardiogram of the baby and child

This diagnostic test for CHD needs a certain kind of ultrasound machine and a trained operator. This is a very big challenge in India. Due to an unfortunate fall out of the Pre-Conception and Pre-Natal Diagnostic Techniques Act, 1994 trained doctors are unable to use portable echocardiogram machines to travel to peripheral hospitals and smaller units who do not have their own machines. Hence, even if there is a suspicion of a CHD in a newborn in these peripheral places, it becomes challenging to perform an echocardiogram.
- Access to Specialized Centres providing heart disorder treatment
As outlined above, there is a big scarcity of centres and also of trained personnel in India. To add to this scarcity, ferrying a sick baby to such a centre is also risky. There is a lack of well-equipped and affordable emergency vehicles to bridge the path to rural areas and centres situated in urban centres.
- Public Perception
Young couples are advised by well-meaning family members and neighbours and often misguided. “The hole will close off on its own” or “wait until baby is 5kg” or “the baby will suffer as a heart patient throughout his/her life” or “try alternative medicine” are common statements made by them. These are incorrect and lead to worsening of the baby’s health as delay can lead to increased morbidity and mortality.
- Finances
Last but not the least, when it comes to interventions in babies, they understandably cost a lot of money. Parents of affected babies are young, likely new (or recent) job holders or have little savings. The insurance companies do not cover any defect occurring prior to birth. So the parents have little options. Government schemes (Pradhan Mantri Yojana, Rashtriya Bal Swasthya Karyakram, Mahatma JyotiBa Phule Yojana, Yashaswini) come to the rescue of below the poverty line card holders. Religious trusts, private companies (CSR) and special NGOs like Genesis foundation dedicated to children with CHD lend a vital helping hand. They also help in raising awareness about CHD.
CHD during Covid-19
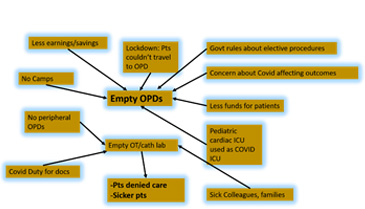
Covid has been brutal to children with CHD, as everything about their care has been impacted. From access to echocardiogram, to pediatric cardiac OPDs, to finances, to open operating theatres, postponed cases and complications of Covid infection. There is now an even greater list of pending cases for pediatric cardiac units to handle in India.
[1] Saxena A. Congenital Heart Disease in India: A Status Report. Indian Pediatr. 2018 Dec 15;55(12):1075-1082. PMID: 30745481.
Dr. Swati Garekar is an American board trained Pediatric Cardiologist from the Children’s Hospital of Michigan. She is a Consultant Pediatric Cardiologist at our hospital partner Fortis Hospital, Mulund, Mumbai. With many years of experience and expertise, she diagnoses and manages babies and children with heart defects. Moreover, she has various publications to her credit.

