The Healer’s Journal: A leaf from my log book
December 23, 2021 | Contributed by Dr Srinivas L
As a doctor working for heart disorders in children, a routine mid-morning at the pediatric cardiac ICU translates to beeping, well ventilated and air-conditioned cubicles, beds with the little babies lying, all the nurses and doctors in level two PPE kits and double face masks.
 Dr Srinivas with his team
Dr Srinivas with his team
Suddenly an 8-month-old boy, who has just come out of sedation and is recovering from anesthesia, begins to cry, breaking the quiet. The child is bawling and his howling echoes are audible till the corridor. His mother, in her early 20s, clad in a PPE suit, is smiling from under the mask and we can see her eyes moist with joy. A rather unusual situation to see a mother smile while her child cries.
Out of sheer curiosity, I ask her, ‘How are you happy that your son is crying?’ and her reply is a reminder of a mother’s pure love. She says, ‘I have never seen my guddu (hindi for baby) cry so loudly ever! In the past he never had the energy to cry continuously.’
Witnessing rebirth
For this little boy, this moment was nothing short of his second birth!
Less than two hours prior to him entering the pediatric cardiac ICU, our anesthetist was doing a cardiac massage (chest compression) on him because he was pulseless on the Cath table. His heart had arrested briefly; to be precise, for a full two minutes. The gentle fingers of our anesthetist were trying to provide the essential pumping action of the heart as it had ceased to beat.
The medical marvel of an emergency Balloon Pulmonary Valvotomy (BPV) performed on a still heart, and now the little boy was crying for a chocolate, as his mother smiled thanking the Gods above for letting her son live.
Standing there, I could feel the gravity of the situation because as the one operating on him, I knew that the little boy had escaped death and emerged a CHD warrior.
Meeting the family
It was only a day prior to the surgery that I’d met this family for the first time in the OPD. The child’s father, in early 20s, barely looked educated, and was a farm laborer from the Beed district, an economically backward region of Maharashtra. The family lives hand to mouth during good seasons of employment and any natural calamity rattles the very basics of their existence.
I could not dare to ask them how they were surviving the Covid-19 pandemic because I did not have the guts to hear what would come out of their mouth. With most of the underprivileged population of our country going through an existential crisis, I restricted my questionnaire just to the medical history.
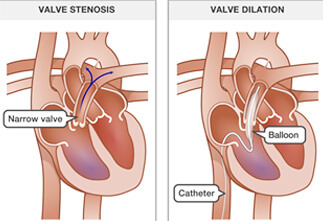
This baby had been diagnosed with severe pulmonary stenosis soon after birth. It is a condition of the heart where a severely narrow heart valve does not allow blood to freely pass from the right ventricle of heart to the lungs.
Had I seen this baby a few months back, I would have advised an emergency cardiac procedure then and there itself. Because being a doctor and a man of science, I’d say it’s miraculous that the baby had survived for 8 months!
His parents told me that he hardly ever plays, struggles to breathe, sleeps little, is constantly in distress, and even struggles to feed!
As a Pediatric Cardiologist working with heart disorders in children, I understand all these symptoms mean that the heart’s working capacity is barely enough to support mere survival and any additional “work” like feeding is not supported by this heart and lungs.
 The child with his mother after surgery
The child with his mother after surgery
Their son’s right ventricle had “failed” and was hardly pumping any blood across the lungs and even his left sided ventricle which pumps blood to the entire body was nearly empty. For the treating team there were several challenges to perform this surgery, so I counseled the parents about the risks involved, as best as I could. Though they were unable to comprehend the criticality of illness and need for the high risk procedure completely, they still consented to death on the table.
The next challenge was arranging funds on an urgent basis for this surgery. I quickly connected with the Foundation dealing with heart disorders and got swift approvals from Genesis Foundation. Luckily the Covid-19 test was negative too, so we could proceed for surgery.
Day of the surgery
Me and my team went through all the steps on how to go about the procedure. My standing instruction was that even if the baby has a cardiac arrest, we do not stop the procedure. We had to complete it because it was the only way to save him.
After a huddle and a prayer, the baby was welcomed into the Cath lab, where such BPV procedures are performed. While trying to pass a wire through the narrow valve, it resulted in complete blockage of any blood flow to lungs and the child had arrested.
But this was expected and there is simply no place for panic in my line of work.
 The process of Balloon Pulmonary Valvotomy
The process of Balloon Pulmonary Valvotomy
Immediately chest compression was started, while the wire position was kept secured. Initially a small balloon was taken across, and the valve was dilated enough for a larger balloon to pass. The procedure was repeated with a larger balloon, while the chest compression continued.
The heart had stopped functioning for 120 seconds, but as soon as the second balloon dilatation was done, everything settled. It was as if there was nothing wrong with the heart!
All his vital signs jumped back to normal, and the beeps of pulse oximeter and the ECG sounded like melody to my ears.
And by the grace of God almighty, this baby went home the next day!
It was a moment of pride and joy for the team.
With a simple procedure, this baby will go on to lead a healthy life now. I can’t say the same for all my patients, but this one is cured and can be cared for like any normal baby without the need of any further cardiac intervention in future. This is the reason I became a pediatric cardiologist because I work to give life a chance for every child who comes to me.
But surgeries like these are not successful without a team who works at the same pace as the doctor. From Beed to the Cath Lab of Jupiter Hospital was possible because of my team and Genesis Foundation, dealing with heart disorders supporting as many underprivileged children as possible.
Dr Srinivas L is a Pediatric Cardiologist at our partner hospital, Jupiter Hospital in Mumbai. With over 22 years of experience, he specializes in correcting Congenital Heart Defects.

